Can Technology Fix Medicine?

After decades as a technological laggard, medicine has entered its data age. Mobile technologies, sensors, genome sequencing, and advances in analytic software now make it possible to capture vast amounts of information about our individual makeup and the environment around us. The sum of this information could transform medicine, turning a field aimed at treating the average patient into one that’s customized to each person while shifting more control and responsibility from doctors to patients.
The question is: can big data make health care better?
“There is a lot of data being gathered. That’s not enough,” says Ed Martin, interim director of the Information Services Unit at the University of California San Francisco School of Medicine. “It’s really about coming up with applications that make data actionable.”
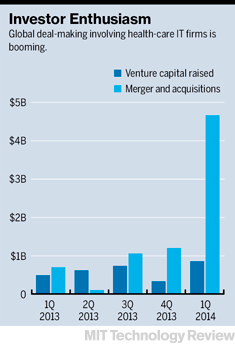
The business opportunity in making sense of that data—potentially $300 billion to $450 billion a year, according to consultants McKinsey & Company—is driving well-established companies like Apple, Qualcomm, and IBM to invest in technologies from data-capturing smartphone apps to billion-dollar analytical systems. It’s feeding the rising enthusiasm for startups as well. Venture capital firms like Greylock Partners and Kleiner Perkins Caufield & Byers, as well as the corporate venture funds of Google, Samsung, Merck, and others, have invested more than $3 billion in health-care information technology since the beginning of 2013—a rapid acceleration from previous years, according to data from Mercom Capital Group.
This MIT Technology Review Business Report looks at the technologies and companies most likely to survive the boom and the challenges they will face as they push to remake health care.
The groups that control the most medical data today are insurance companies and care providers, and their data analysis is already beginning to change health care. Express Scripts, which manages pharmacy benefits for 90 million members in the U.S. and processes 1.4 billion prescriptions a year, has scoured its data from doctors’ offices, pharmacies, and laboratories to detect patterns that might alert doctors to potential adverse drug interactions and other prescription issues. Doctors can now know 12 months in advance, with an accuracy rate of 98 percent, which of their patients may fail to take their medicine. Taking steps to avert that problem could improve patients’ health and reduce the $317 billion spent in the United States each year on unnecessary ER visits and other treatment.
Today many companies and health-care providers are adding other layers of information to create an increasingly precise, patient-specific brand of medicine. New mobile technologies, for example, could provide information about a patient’s everyday behaviors and health, creating opportunities for care providers to influence patients far more frequently. Data brought in from electronic health records would add doctors’ insights, test results, and medical history. Genetic data would offer insight into whether patients are predisposed to certain conditions or how they might react to treatments.
“We want to believe that most of the things we do in medicine are based on evidence,” says Malay Gandhi, managing director of Rock Health, which funds health-care startups. “Some are, but most aren’t.” The opportunity, he says, is that medicine could become more analytical and evidence-based.
Data is also changing the role of patients, offering them a chance to play a more central part in their own care. One way is by using mobile technology to monitor sleep patterns, heart rate, activity levels, and so on. In development are even more advanced devices capable of continuously monitoring such key metrics as blood oxygen, glucose levels, and even stress. And companies like Apple are hoping to become repositories for all this information, giving consumers new ways to track and perhaps improve their health.
This kind of information may be useful and interesting for anyone, but it can become essential for the millions living with chronic conditions like diabetes, heart disease, and depression. WellDoc makes a prescription-only FDA-approved “patient coaching” system, which advises users on how much insulin they should take in light of information recorded on their smartphones: blood sugar levels, recent meals, and exercise. It also offers tailored messages of encouragement and provides the patient’s doctor with treatment recommendations based on the data and established medical guidelines. A feature under development would enable the system to predict a hypoglycemic reaction and help users avoid it.
Ginger.io uses data collected (with permission) from a phone and other sensors to assess the behavior of people with mental illnesses such as depression. Are they calling loved ones, or getting enough sleep? When a patient is showing signs of struggling, someone can be alerted.
Over time, both companies will aggregate this information to help doctors study and improve treatment overall. “It’s like one of the largest clinical trials in history,” says Chris Bergstrom, WellDoc’s chief strategy and commercial officer. “And it’s not even in an artificial environment—it’s in real time.”
Families affected by Phelan-McDermid syndrome, a rare condition in which a deletion on chromosome 22 causes problems such as learning and memory deficits, are building a database of information from genomic tests, clinical medical records, extensive family surveys and histories, and more. The goal is to create a central repository where researchers can examine multiple sources of data simultaneously. That’s increasingly important as researchers begin to see connections between Phelan-McDermid, autism, and other conditions. Another benefit: data that once would have been locked up in one academic researcher’s lab will now be readily available to many different experts.
“So much of that data is already out there,” says Megan O’Boyle, whose daughter Shannon was diagnosed in 2001, just two years after chromosome 22 was sequenced. “It’s just sitting there waiting to be used.”
Keep Reading
Most Popular
Large language models can do jaw-dropping things. But nobody knows exactly why.
And that's a problem. Figuring it out is one of the biggest scientific puzzles of our time and a crucial step towards controlling more powerful future models.
The problem with plug-in hybrids? Their drivers.
Plug-in hybrids are often sold as a transition to EVs, but new data from Europe shows we’re still underestimating the emissions they produce.
Google DeepMind’s new generative model makes Super Mario–like games from scratch
Genie learns how to control games by watching hours and hours of video. It could help train next-gen robots too.
How scientists traced a mysterious covid case back to six toilets
When wastewater surveillance turns into a hunt for a single infected individual, the ethics get tricky.
Stay connected
Get the latest updates from
MIT Technology Review
Discover special offers, top stories, upcoming events, and more.