Gene-Therapy Grafts Have Repaired a Child’s Devastating Skin Disorder
In June 2015, a seven-year-old boy was admitted to a burn unit at a hospital in Germany, not for a burn but for blisters that covered almost his entire body. They were caused by a severe genetic illness—a connective tissue disorder called epidermolysis bullosa.
He had lost about 60 percent of the outer layer of his skin, which led to a life-threatening bacterial infection. To save his life, doctors performed an experimental procedure that involved taking healthy skin cells from the patient’s body, genetically modifying them in a lab, and growing the cells into sheets that they then grafted onto his body.
Using this technique, known as gene therapy, researchers were able to reconstruct 80 percent of the boy’s skin, including his arms, legs, and back. The treatment is detailed today in the journal Nature.
Small patches of skin had been repaired this way before, but Jean Tang, a physician and associate professor of dermatology at Stanford, says this is the largest amount of skin that has been reconstructed by gene therapy to date. Tang and her colleagues, along with biotech company Abeona, are working on a similar approach for another type of epidermolysis bullosa. There are three main types of the disease, which can be caused by inherited mutations in different genes.

Patients with epidermolysis bullosa live in excruciating pain, their skin so fragile to the touch that those born with the disorder have been nicknamed “butterfly children.” The disorder produces chronic and untreatable wounds that get infected easily and can eventually become cancerous. About 500,000 people worldwide have epidermolysis bullosa.
In this study, the patient’s cells contained a mutation in the LAMB3 gene, which affects a protein needed to strengthen the epidermis, the top layer of the skin, and help it attach to underlying layers. Mutations in this gene make abnormal proteins that cause the skin to blister, eventually forming open, chronic wounds.
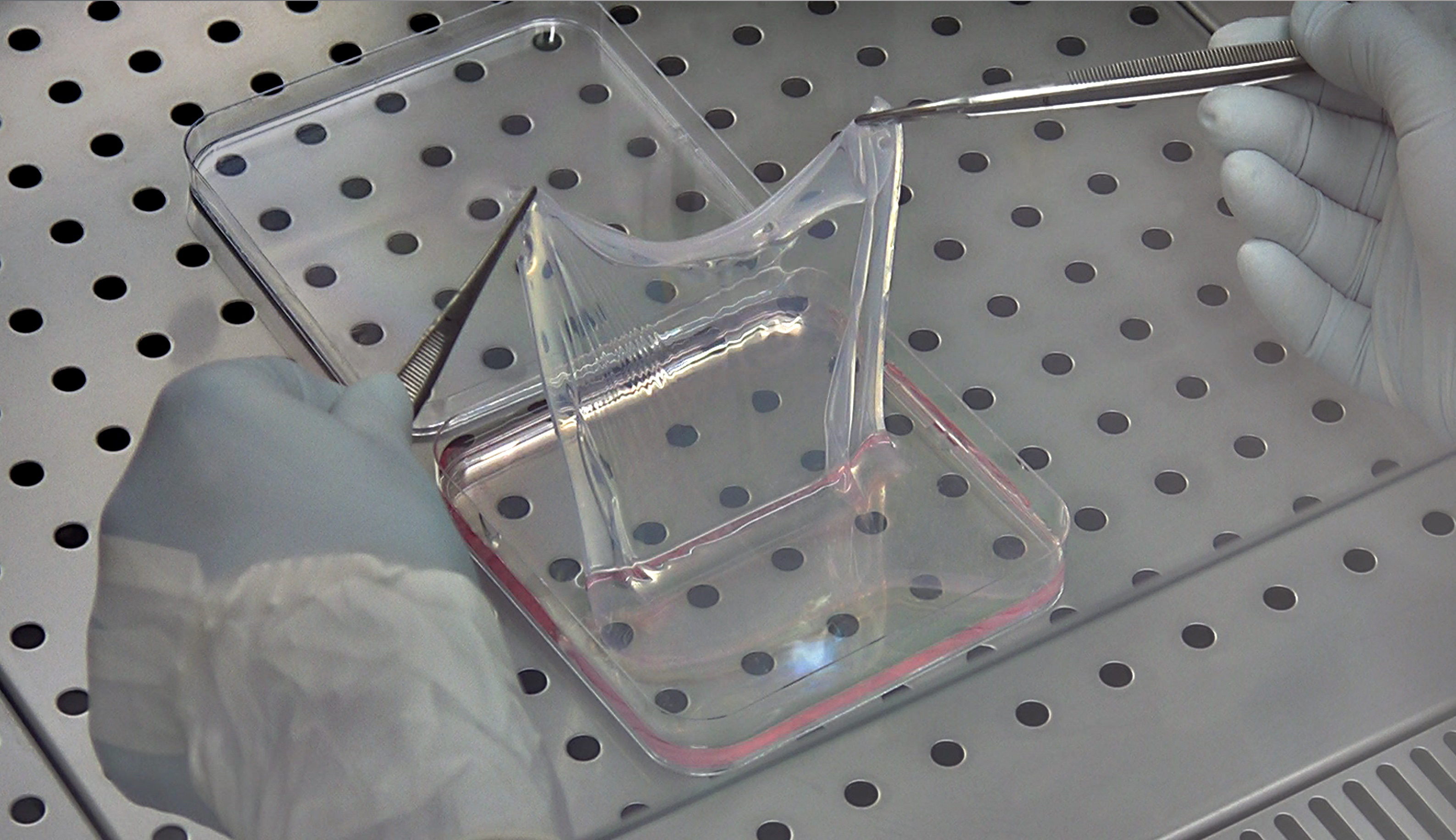
Researchers extracted cells from a non-blistering area of the child’s body. From this skin sample, they isolated stem cells, which have the ability to regenerate new, healthy skin cells. To correct the genetic mutation, they treated the patient's cells with an engineered virus containing a correct copy of the LAMB3 gene. They grew more of these cells into sheets and then grafted them onto the patient’s body. The sheets ranged in size from two by three inches to about five by five inches.
The grafts were applied in a series of three surgeries. The skin has since healed normally, with no blisters in the reconstructed areas, and the child has been able to return to school and even play soccer.
Tang says she is “extremely excited” about the results. She and her colleagues are using skin grafts to treat and heal chronic open wounds, but not to replace the entire skin.
One of the study’s authors, Michele De Luca of the University of Modena and Reggio Emilia in Italy, says he doesn’t think there will be a need to reapply the grafts over time.
“If we think about the experience we have with burns, this epidermis will stay basically forever,” De Luca said Tuesday in a call with journalists. Doctors have treated burn patients with skin grafts that have lasted for more than 30 years, he said. In other words, this could be a one-time cure for the disease.
Brett Kopelan, executive director of the nonprofit Dystrophic Epidermolysis Bullosa Research Association of America, says gene therapy looks like the best hope for the disease, which currently has no cure. Kopelan’s 10-year-old daughter has a severe form of the disorder.
“This would completely change her world,” he says. “You’re talking about an entirely new life.”
Keep Reading
Most Popular
Large language models can do jaw-dropping things. But nobody knows exactly why.
And that's a problem. Figuring it out is one of the biggest scientific puzzles of our time and a crucial step towards controlling more powerful future models.
The problem with plug-in hybrids? Their drivers.
Plug-in hybrids are often sold as a transition to EVs, but new data from Europe shows we’re still underestimating the emissions they produce.
Google DeepMind’s new generative model makes Super Mario–like games from scratch
Genie learns how to control games by watching hours and hours of video. It could help train next-gen robots too.
How scientists traced a mysterious covid case back to six toilets
When wastewater surveillance turns into a hunt for a single infected individual, the ethics get tricky.
Stay connected
Get the latest updates from
MIT Technology Review
Discover special offers, top stories, upcoming events, and more.